Consult and History
 When a patient comes in for the first time, we spend a long time reviewing their situation and discussing their past. What treatment did they have in the past? What is their medical and sexual history? What financial, emotional, or other non-medical barriers got in their way? What do they want for a successful outcome?
When a patient comes in for the first time, we spend a long time reviewing their situation and discussing their past. What treatment did they have in the past? What is their medical and sexual history? What financial, emotional, or other non-medical barriers got in their way? What do they want for a successful outcome?
These questions need answers from both partners. More often than not, each partner has different answers, and we all need to get on the same page before going ahead with the process.
We also want to know what steps the couple has already taken on their own to enhance their fertility. Have you done any home testing for ovulation, cervical mucus, sperm health, or hormone levels? All of this information can help me know your history in better detail.
Tests
 The first “test” we conduct is a physical examination. We look for obvious physical problems that might impact overall health. At Gold Coast, we have diagnosed my share of breast and cervical cancer, diabetes and blood disorders, kidney disease and TB, though the doctors here are not general physicians or OB/GYNs. But our physical exam is thorough and designed to evaluate your overall reproductive health.
The first “test” we conduct is a physical examination. We look for obvious physical problems that might impact overall health. At Gold Coast, we have diagnosed my share of breast and cervical cancer, diabetes and blood disorders, kidney disease and TB, though the doctors here are not general physicians or OB/GYNs. But our physical exam is thorough and designed to evaluate your overall reproductive health.
We will also conduct a vaginal ultrasound during this exam, to see what your ovaries and uterus look like. Again we can often discover obvious physical reasons for your infertility, such as blocked tubes, an abnormal uterus, or scarred ovaries.
In addition to the physical exam we conduct a battery of lab tests that give us important information about your reproductive health:
- Tests to measure your hormone levels
- Tests to measure your ovarian reserve (the clomid challenge)
- Tests to measure your prolactin and thyroid function
- I may do a pap smear to make sure you do not have an infection or abnormal findings
- Tests for Autoimmune diseases, like diabetes, lupus, or RA
Depending what we find in ultrasound, we might do other imaging tests to give us more data before we make a diagnosis. We might do a special ultrasound called an SHG to see if your tubes are clear. We might also do an exploratory laparoscopy (microsurgery) to see if you have endometriosis or scarring. Hysteroscopy, a type of microsurgery, gives us direct access to the uterus to visualize disease better.
Another test is called HSG, where we insert dye through the cervix into the uterus and fallopian tubes. This test will show us if there are blockages or abnormalities anywhere, and give us a lot more information about tumors, structural abnormalities, polyps, or other factors that might be causing your infertility.
Diagnosis
After all of this testing, combined with what we’ve learned about your history and your goals, we will have the information we need to formulate a diagnosis. Remember, infertility is a complex, multi-level disease, and no two cases are alike. The diagnosis might reflect a number of different barriers you face to pregnancy, including infertility affecting your partner.
Treatment Plan
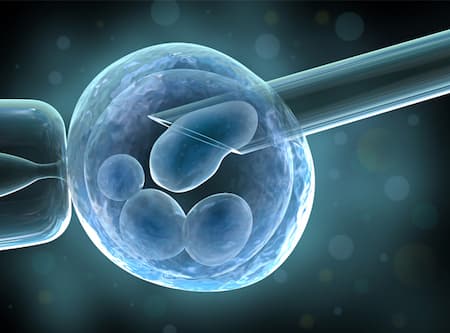 You and your doctor will sit down together after we reach a diagnosis and make a plan for achieving your goals. Depending on how much urgency we have time wise, we will have more than one choice of treatment. Watch out for doctors that treat all infertility with the identical treatment. IVF is not the answer for every patient, neither is clomid and insemination. You might need surgery, hormone treatment, IVF or other interventions. No matter what the cause of your infertility, you will have a pathway to success.
You and your doctor will sit down together after we reach a diagnosis and make a plan for achieving your goals. Depending on how much urgency we have time wise, we will have more than one choice of treatment. Watch out for doctors that treat all infertility with the identical treatment. IVF is not the answer for every patient, neither is clomid and insemination. You might need surgery, hormone treatment, IVF or other interventions. No matter what the cause of your infertility, you will have a pathway to success.
Even if our initial attempts at treatment don’t give us a successful outcome, each try gives us valuable information that cycles right back into my diagnosis process. This is where the Fertility Audit makes a big difference: we keep repeating the diagnostic cycle until our treatment plan succeeds. With each test, each attempt to conceive, we get more information about your personal situation and can craft a personalized treatment plan that takes into account your constellation of needs, and how your body personally responds to treatment.
 When a patient comes in for the first time, we spend a long time reviewing their situation and discussing their past. What treatment did they have in the past? What is their medical and sexual history? What financial, emotional, or other non-medical barriers got in their way? What do they want for a successful outcome?
When a patient comes in for the first time, we spend a long time reviewing their situation and discussing their past. What treatment did they have in the past? What is their medical and sexual history? What financial, emotional, or other non-medical barriers got in their way? What do they want for a successful outcome? The first “test” we conduct is a physical examination. We look for obvious physical problems that might impact overall health. At Gold Coast, we have diagnosed my share of breast and cervical cancer, diabetes and blood disorders, kidney disease and TB, though the doctors here are not general physicians or OB/GYNs. But our physical exam is thorough and designed to evaluate your overall reproductive health.
The first “test” we conduct is a physical examination. We look for obvious physical problems that might impact overall health. At Gold Coast, we have diagnosed my share of breast and cervical cancer, diabetes and blood disorders, kidney disease and TB, though the doctors here are not general physicians or OB/GYNs. But our physical exam is thorough and designed to evaluate your overall reproductive health. You and your doctor will sit down together after we reach a diagnosis and make a plan for achieving your goals. Depending on how much urgency we have time wise, we will have more than one choice of treatment. Watch out for doctors that treat all infertility with the identical treatment. IVF is not the answer for every patient, neither is clomid and insemination. You might need surgery, hormone treatment, IVF or other interventions. No matter what the cause of your infertility, you will have a pathway to success.
You and your doctor will sit down together after we reach a diagnosis and make a plan for achieving your goals. Depending on how much urgency we have time wise, we will have more than one choice of treatment. Watch out for doctors that treat all infertility with the identical treatment. IVF is not the answer for every patient, neither is clomid and insemination. You might need surgery, hormone treatment, IVF or other interventions. No matter what the cause of your infertility, you will have a pathway to success.