Blocked Tubes & Surgery
 Sometimes the barrier to pregnancy is a physical one: your fallopian tubes, blocked by scar tissue. But is surgery the only answer?
Sometimes the barrier to pregnancy is a physical one: your fallopian tubes, blocked by scar tissue. But is surgery the only answer?
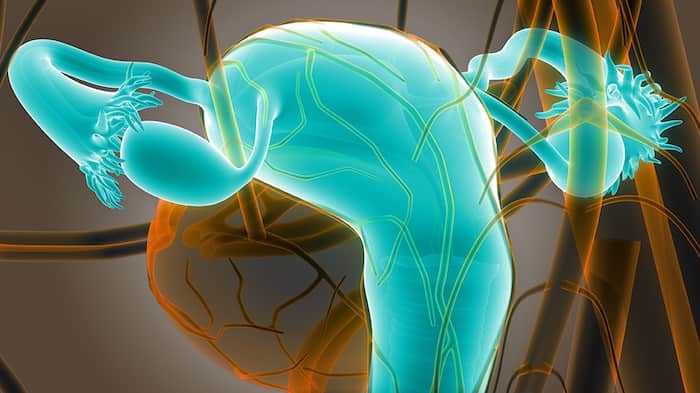
Endometriosis is only one reason your fallopian tubes might become blocked due to scarring. Why are scarred fallopian tubes important to your fertility? Remember how the process works – the egg gets fertilized by the sperm in the tube, and then the fertilized egg travels down the tube into the uterus where the zygote implants and pregnancy begins.
A sperm can’t make it through a blocked tube. Even worse, if a sperm manages to make it through and fertilize the egg, if the egg can’t make it into the uterus the whole process is for nothing – the fertilized egg never implants and grows. Or even worse, the fertilized egg will implant in the tube, causing a catastrophic condition called an ectopic pregnancy. The tube can’t carry a pregnancy, and if it goes untreated by medicine or surgery, an ectopic can rupture, causing destruction to your reproductive system or even death of the mother!
So how does this happen? How do tubes get blocked in the first place?
- Endometriosis – I’ve mentioned this disease before here. Endometrial tissue develops outside the uterus, causing pain, bleeding and scarring. If it happens in your tubes, the scarring can block your tubes
- STD Infections – Infections from STDs like chlamydia and gonorrhea can scar your tubes and/or your uterus. Often these STDs have no symptoms but leave lifelong effects in your reproductive system. Also, I have treated a number of women from China, India, and other countries where they had tuberculosis in their uterus and tubes, causing massive scarring. If you are from another country where TB infections are more common, or if you live in an area of the US where lots of people come from other countries, be aware that TB is a possibility
- Surgery or medical treatments – Surgeries to treat another condition, such as appendicitis, can also cause scarring to your tubes as a side effect of your surgery. You might also get scarred tubes after treatment for a disease like cancer or operations to remove tumors or other disease.
- Having your tubes “tied” in the past – You might have gotten your tubes “tied” as a form of birth control and want to reverse that procedure and reattach the tubes. Surgery might be able to reverse the procedure, depending on how the procedure was done and the skill of the surgeon.
So, it sounds like surgery is the obvious answer to these problems, right? Open the tube and fertility will follow?
The answer is a definite maybe. To find out the truth, know your history, get an accurate diagnosis, and make a treatment plan that addresses the root causes of your infertility.
- Step 1: Know your history (of disease, of pain, of prior diagnoses from other doctors) and share that history with a qualified reproductive endocrinologist.
- Step 2: Get a thorough work up and have a doctor that will look at the tests and results to make an accurate diagnosis. Here is a list of some of the tests, again, that we use to diagnosis tube blockage as a contributor to infertility:
- HSG – hysterosalpingogram (x-ray of your tubes)
- SGH – sonohysterogram (ultrasound of your tubes)
- diagnostic laparoscopy or falloposcopy
- hysteroscope
- Step 3: Once the diagnosis is in place, make a treatment plan. If surgery is part of the plan, here are the surgical options:
- laparoscopy – minimally invasive surgery or keyhole surgery where they go through a tiny incision below your belly button with a tiny scope and surgical tools. Leaves minimal scarring and much faster recovery time *laparotomy – “open” surgery, traditional style where they open you up. This is a major abdominal surgery done this way.
- robot surgery – a new surgical technique where robot technology enhances the reach of a laparoscopy. Can get you amazing results if your surgeon is experienced in using robotic techniques.
Now, even after surgery you might have an increased risk of an ectopic pregnancy. Or the surgery itself might lead to scarring. Every single case is different, which is why you want to choose your partner in care with some thought behind the choice.
- Step 4: Assess how the surgery went and make a plan to proceed to pregnancy If the surgery was a brilliant success and the tubes are completely unblocked, you might be able to conceive naturally now, as long as no other infertility factors are present and your partner has his own fertility in order, with motile, healthy, plentiful sperm.
- But surgery isn’t a panacea. Sometimes the tubes are so damaged, part of a larger pattern of scarring in your whole abdomen, that saving the ovaries that produce the eggs is the main goal. As long as at least one ovary is saved, you can continue to produce eggs. If surgery cannot completely restore your tubes, you will need to go through IVF, where you take an egg, fertilize it in a dish with your partner’s sperm, and carefully insert it into the right place in your uterus for implantation.
- In addition, as I mentioned, you might have increased risk of tubal pregnancy (ectopic) after tubal surgery. I have seen cases of heterotopic pregnancy, where one egg implants normally in the uterus and another, in the same cycle, implants in the tube! This is a life threatening and easy to miss condition, so if you have sudden pain, bleeding, nausea, or faintness during your early pregnancy it’s important to contact your doctor right away to rule out ectopic or heterotopic pregnancy.
- But back to the process of deciding on whether or not to do tubal surgery in the first place! Now, if the tests show that you have widespread scarring in your tubes, if you don’t have pain I might recommend that you skip the surgery and go right for IVF if speed and quicker success is your highest priority. If you are suffering from pain, surgery might be crucial even if the goal isn’t to save your tubes but an ovary if possible. If we can stop pain resulting from scarring, you can still get pregnant via IVF even if your tubes have been removed.
- Finally, if your blocked tubes are filled with fluid (hydrosalpinx) you will have to treat this condition even if you decide to go straight to IVF. The fluid will interfere with the success of IVF so you have to treat these kinds of blocked tubes surgically before going to IVF to treat your infertility.
To sum up…
 Surgery is one tool a reproductive endocrinologist has to treat tubal blockages. But you are not just your tubal disease. Tubal disease is only one piece of a bigger picture. Your age, other fertility factors, your partner’s fertility, and the cause, extent, and type of tubal disease will all impact the decision making process. Every case is different. As a patient, you can increase the likelihood of success by giving your doctor all the clues you have as to your tubal disease, follow through on all testing so that you have the most information to make an informed decision, then factor in your personal decisions about your priorities before going ahead with surgery.
Surgery is one tool a reproductive endocrinologist has to treat tubal blockages. But you are not just your tubal disease. Tubal disease is only one piece of a bigger picture. Your age, other fertility factors, your partner’s fertility, and the cause, extent, and type of tubal disease will all impact the decision making process. Every case is different. As a patient, you can increase the likelihood of success by giving your doctor all the clues you have as to your tubal disease, follow through on all testing so that you have the most information to make an informed decision, then factor in your personal decisions about your priorities before going ahead with surgery.
Some questions you might need to answer before you can make a plan:
- How much pain am I suffering due to the scarring? Can I treat the pain and improve my fertility at the same time by repairing the tubes instead of removing them?
- Are my ovaries in danger? If I can save an ovary or both ovaries, is IVF a good option for me?
- Am I ready to go ahead and conceive naturally, even at the increased risk of a tubal pregnancy?
One of the things that makes infertility such a challenge for patients is the complexity of the disease and the multi-level decision-making process that you have to take to navigate the barriers to pregnancy. But we can help you navigate all these challenges!